Optometry’s New Frontier; Setting An Improved Standard of Care for AMD
By Dr. Victoria Dzurinko, OD, MBA, FAAO
Writing a new narrative on AMD management.
Optometrists have been in the business of preventative medicine for decades. Every day we have discussions with our patients about modifiable risk factors including diet changes for diabetes, UV protection for cataract patients, and environmental adjustments for patients with dry eye. Over time, our profession has evolved and been elevated to that of primary eye care providers and, as such, it’s become increasingly important that we diagnose and manage degenerative diseases like glaucoma and AMD.
Reining in glaucoma
Our profession has embraced glaucoma detection and management. We are good at measuring structure and function in these patients. We meticulously pour over VFIs and GPA analyses so that we can intervene promptly when we observe the slightest progression.
The advent of visual field analysis helped set a new standard of care for glaucoma. We know we can’t cure the disease, or completely eliminate the chances that our patient will go blind. We cannot predict how quickly a patient will progress and we are cognizant that managing the disease will likely be a long game. Yet we do not hesitate to treat IOP when perimetry testing indicates early pathology – even in the absence of any clinical signs of disease – to reduce the risk of glaucomatous optic neuropathy in the future. Ultimately, we want to intervene before our patients experience any debilitating vision loss and the integration of functional testing has enabled us to do what is best for our patients.
The status quo of AMD care
Much like glaucoma, AMD is a chronic, progressive disease that starts years before the first physical signs are evident using current imaging technology.
Unlike glaucoma, pathological progression of AMD is particularly insidious and vision loss can happen quickly. Patients may have a BCVA of 20/20 and no obvious indication of the disease, except having trouble seeing in the dark. As with presbyopia, they attribute night blindness to “getting old” and consider it a “normal part of aging.” They stop driving at night. They start planning social activities around being home before dark. They may not think to report this to us as a health concern until their visual acuity declines, at which point disease progression is well under way and may be harder to manage.
Up until now, we have stood relatively hopelessly on the sidelines taking pictures and scans as our patients have progressed. Sometimes we are able to visualize the earliest signs of neovascular proliferation and intervene as soon as possible—but timely treatment can only happen if we are lucky enough to detect these changes before the patient presents with severe vision loss.
There has to be a better way to detect and manage AMD.
Making a case for functional testing for AMD
Understanding the effects of a disease state on both the structure and function of an organ is vital to early intervention and optimal outcomes. It is a concept that is accepted standard of care in glaucoma management, but not yet in AMD. We are comfortable addressing and treating glaucoma, a typically slow progressing disease, at the first sign of functional impairment; yet we have been slow to do the same for AMD, knowing it could rob a patient’s vision overnight.
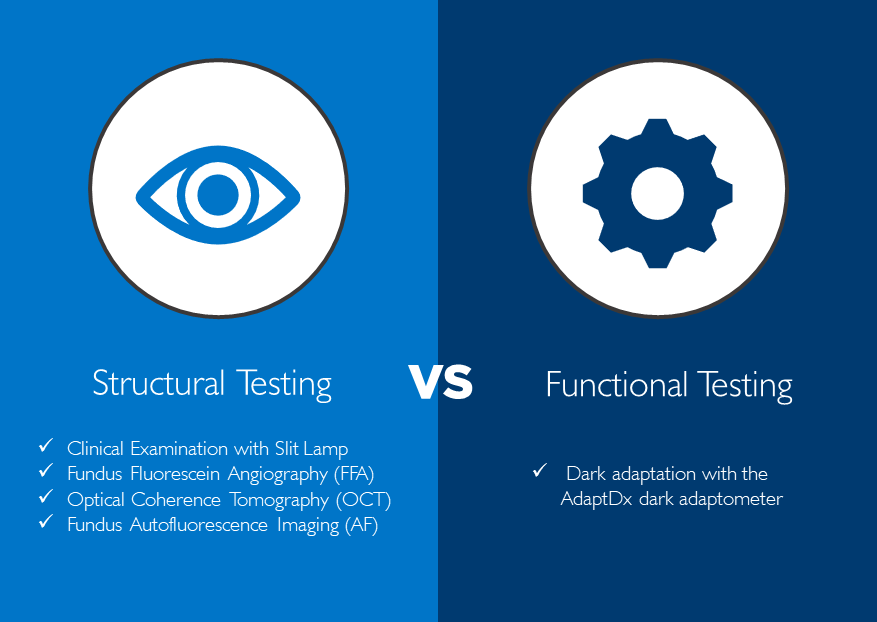
Those of us on the front line of primary eye care need to write the new narrative on AMD detection and management. Much like visual field analysis did for glaucoma, the technology exists today to move us beyond observing structural changes in AMD. AdaptDx® is a device that provides an objective assessment of retinal function that clearly identifies dark adaptation impairment – the very first biomarker of AMD – and makes it possible to monitor disease progression. The simple, automated results generated by the AdaptDx are 90% specific and sensitive to AMD. It provides the ability to detect functional impairment resulting from underlying pathologies that precede clinical presentation of the disease, as well as the means to closely monitor disease progression.
Starting today, we can switch from being reactive observers of AMD to being active fighters of this disease. Integration of dark adaptation testing into clinical practice expands diagnostic capabilities to accurately detect and effectively manage AMD. With a promising future, adoption of the technology has great potential to improve patient care and clinical outcomes.
Let us set a new standard of care for AMD. By diagnosing the disease at its earliest stages via functional testing, we can work with our patients to help them avoid severe vision loss and disability. Together, we can work to protect the retina and allow patients to live their best and most active lives for many years to come.
Best regards,
![]()
Primary eye care conquered glaucoma because they use technology that enabled them to accurately diagnose and monitor the disease.
 Gregory Jackson, PhD
Gregory Jackson, PhD

About the Author
Victoria Dzurinko, OD, MBA, FAAO, Associate Director of Professional Relations with MacuLogix, has spent 17 years in optometry in various roles including education, industry consulting, and practice ownership. She graduated from Salus University, completed her residency at The Eye Institute, and earned her MBA in healthcare and pharmaceutical marketing from St. Joseph’s University in Philadelphia. Dr. Dzurinko is excited to help optometrists elevate their standard of care and improve patient outcomes in the management of AMD.
